In the early 2000s, Congressman Jerry Nadler underwent a dramatic health transformation that stirred national attention. Known for his long-standing role in New York politics, Nadler made headlines not for his legislation, but for his decision to undergo bariatric surgery. At a time when weight loss surgery was still emerging in public discourse, Nadler’s openness brought both awareness and scrutiny.
Before surgery, Nadler’s weight had reached 338 pounds. At just 5 feet 4 inches tall, this placed him in the morbidly obese category. Alongside the physical limitations—difficulty walking even short distances—Nadler faced multiple serious health risks: heart disease, diabetes, and breathing problems. His attempts to lose weight through traditional means, including Weight Watchers, liquid diets, and pharmaceutical programs like Fen-Phen, all led to temporary success followed by relapse.
The emotional burden was just as significant. Nicknamed “Jerry Waddler” by critics and subjected to public mockery, Nadler lived under the dual pressure of political visibility and personal discomfort. These cumulative factors prompted a more permanent and medically guided solution.

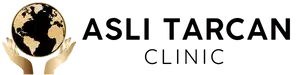
What Type Of Weight Loss Surgery Did He Undergo?
In August 2002, Nadler began the first of a two-stage laparoscopic duodenal switch, performed at Mount Sinai Hospital in Manhattan. A second surgical phase followed in 2003. The duodenal switch, often abbreviated as DS or GRDS (gastric reduction duodenal switch), is among the most complex bariatric procedures available today.
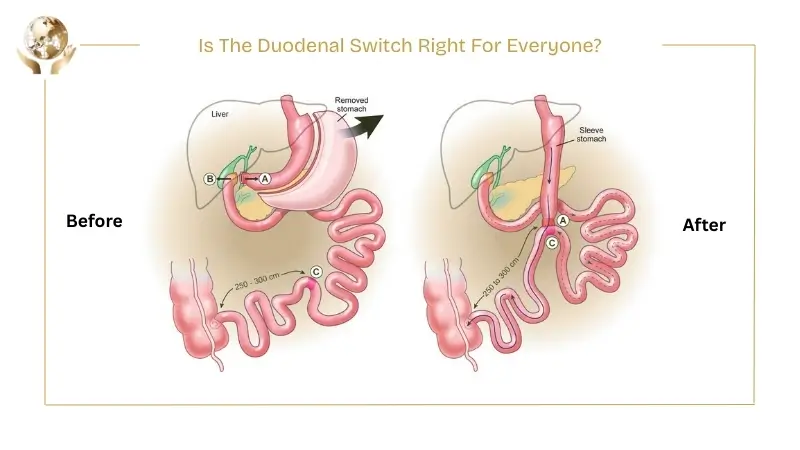
It combines two components:
- Restrictive: Approximately 70% of the stomach is removed, leaving a sleeve-like pouch to limit food intake.
- Malabsorptive: The small intestine is rerouted, creating two separate pathways—one for food, one for bile—before joining in a shortened common channel. This limits calorie and fat absorption.
The malabsorptive nature of the procedure makes it especially effective for patients with severe obesity and obesity-related comorbidities.

How Effective Was The Surgery For Nadler?
Following the first phase, Nadler lost 61 pounds within three months. By July 2003, his total weight loss exceeded 100 pounds. More importantly, his quality of life improved dramatically. He went from avoiding brief walks to comfortably walking 40 city blocks. His meals, once substantial in portion, became small and manageable. The emotional shift—freedom from physical limitation and public ridicule—was just as profound as the physical one.
Though Nadler never disclosed whether he reached his target weight of 160 pounds, the transformation marked a significant turning point in both his health and confidence.
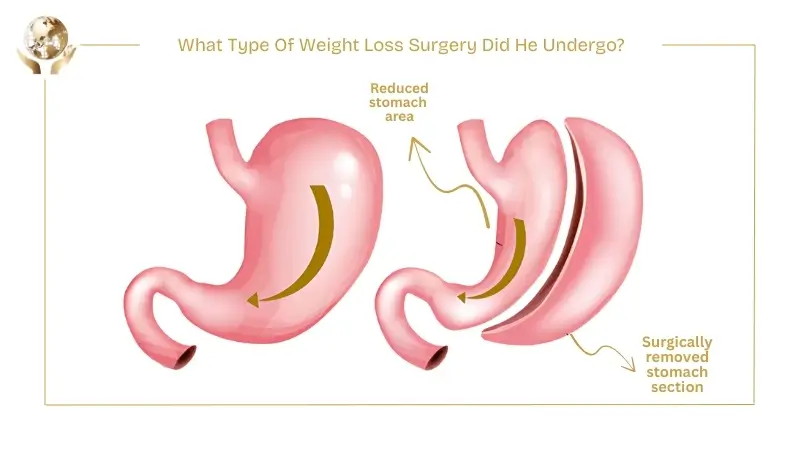
What Risks Are Involved With The Duodenal Switch?
While the duodenal switch offers high success rates in treating obesity and Type 2 diabetes (up to 98% remission), it is not without risks:
Short-term complications may include:
- Perforation of the bowel or stomach
- Infections and abscesses
- Deep vein thrombosis
- Pulmonary embolism
Long-term complications include:
- Vitamin and mineral deficiencies (especially fat-soluble vitamins A, D, E, K)
- Chronic diarrhea and smelly gas
- Internal hernias or bowel obstruction
Patients must commit to lifelong supplementation, including daily multivitamins, calcium citrate, and regular bloodwork to monitor for deficiencies.
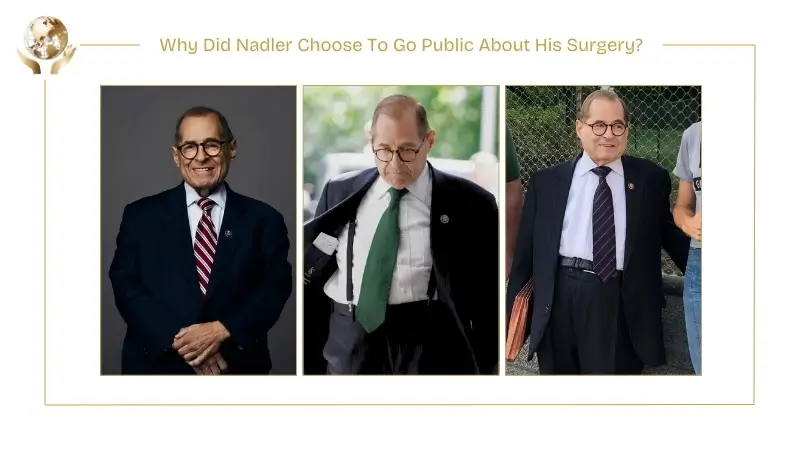
Why Did Nadler Choose To Go Public About His Surgery?
In an age where weight loss procedures were often hidden or stigmatized, Nadler chose transparency. He announced his surgery shortly after undergoing it, citing a desire to control the narrative rather than have it leaked by tabloids. The response was largely positive. Colleagues applauded his courage, and some even described him as an inspiration.
Despite this, public mockery didn’t entirely disappear. Years later, in 2019, then-President Donald Trump referred to him as “Fat Jerry,” illustrating how weight-related stigma can persist, even after dramatic transformation.
What Does Nadler’s Story Teach Us About Obesity And Stigma?
Nadler’s journey reveals the layered nature of obesity—not just as a medical condition, but a social and emotional challenge. His case highlights how severe obesity can impact self-worth, public image, and physical mobility, and how surgery, when chosen carefully, can be a tool for reclaiming health and dignity.
His story also demonstrates that weight loss surgery is not a cosmetic shortcut, but a complex medical intervention with serious risks and lifelong requirements. For those facing similar health concerns, it offers a reminder to seek comprehensive evaluations and support systems.
Is The Duodenal Switch Right For Everyone?
No single surgery fits all. The duodenal switch is typically reserved for individuals with a BMI over 50 or those with severe metabolic disease. It’s not as commonly performed as procedures like the gastric sleeve or bypass, due to its complexity, cost, and nutritional demands. However, for the right candidate, it delivers unmatched long-term results.
Patients considering this surgery should be evaluated by a multidisciplinary bariatric team, and must be prepared for lifelong follow-up.